Recurrent Pregnancy Loss Clinic
|
Many people are able to become pregnant but have trouble carrying a pregnancy to term. Those with this fertility issue, called recurrent pregnancy loss, need and deserve specialized, compassionate care.
At the Northwestern Medicine Recurrent Pregnancy Loss Clinic, we help people become parents by providing exceptional patient care. As part of an academic health system, we offer leading-edge treatment approaches guided by the latest research. The loss of one pregnancy can be physically and emotionally difficult. Experiencing more than one can be even more challenging. That’s why we are committed to offering comprehensive care that addresses both the medical and psychological needs of patients experiencing recurrent pregnancy loss. What is Recurrent Pregnancy Loss? Pregnancy loss is common. In fact, up to 25% of pregnancies end in miscarriage. Recurrent pregnancy loss is defined as losing two or more pregnancies, and it is far less common:
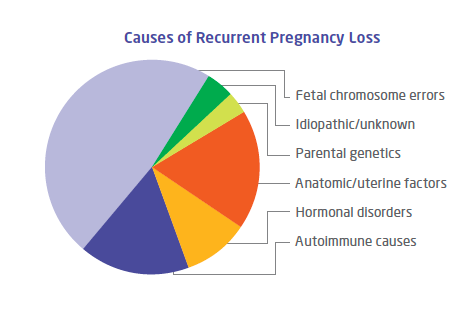
Possible Causes of Recurrent Pregnancy Loss The cause of recurrent pregnancy loss is only known in half of cases. It can be related to genetics, anatomy, hormones or autoimmune disorders. How We Treat Recurrent Pregnancy Loss
At the Northwestern Medicine Recurrent Pregnancy Loss Clinic, we use a multidisciplinary and personalized approach to meet your unique needs. If you have had two or more pregnancy losses, you can schedule a consultation in the clinic. This consultation will be with both a physician and psychologist. At this visit, you can expect to discuss:
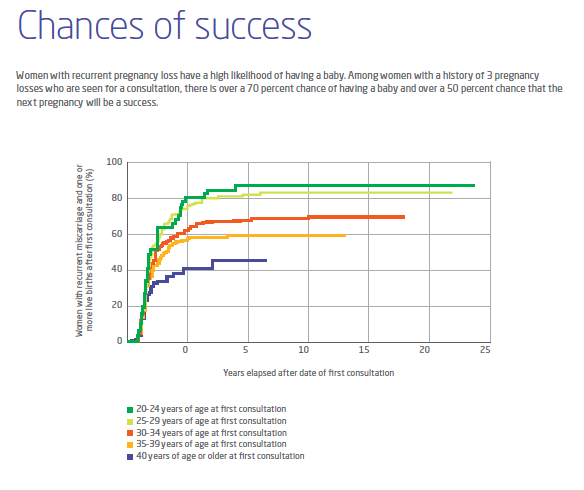
After your consultation, your care team will develop a treatment plan for you. After you or your partner conceives again, the clinic care team will monitor you frequently throughout your first trimester. Near the end of the first trimester, you will return to your obstetric team to continue ongoing prenatal care. We offer mental health counseling through pregnancy and postpartum as well. Outcomes Patients with recurrent pregnancy loss have a high likelihood of having a baby with support from a specialized care team. Data from clinics like ours that specialize in recurrent pregnancy loss show that many women achieve a live birth after receiving care for recurrent pregnancy loss. Meet Our Team
Your care team will consist of physicians, psychologists and nurses who specialize in reproductive endocrinology and infertility. Your multidisciplinary team may also include experts in:
Research
Our team is committed to improving the reproductive outcomes for people with recurrent pregnancy loss. We are constantly working to identify causes, pioneer new evaluation strategies and treatments, and better understand the psychosocial factors that impact those who face this condition. We welcome your involvement to help find answers for those who face recurrent pregnancy loss. To help us identify new causes and treatments, we invite you to participate in our research. Some studies may involve simple questionnaires while others may involve blood tests, uterine tests, sperm tests or new treatments. Participation in research is completely voluntary. If you choose not to participate, it will not impact your care in any way. To learn more or to participate in any of our research projects, please reach out to your Northwestern Medicine physician or our OB-GYN REI clinical research team for more information:
|
Locations & Appointments
We offer access to world-class care, closer to home. Visit us at one of our four locations in the Chicagoland area: Chicago, Geneva, Highland Park, or Oakbrook Terrace. To schedule an appointment, call 312.695.7269 (TTY: 711). Resources
|
References
- The Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of RPL: a committee opinion. Fertil Steril. 2012;98:1103-11.
- Brigham SA, Conlon C, Farquharson RG. A longitudinal study of pregnancy outcome following idiopathic recurrent miscarriage. Hum Reprod. 1999;14:2868-71.
- Lund M, Kamper-Jørgensen M, Nielsen HS, Lidegaard Ø, Andersen AM, Christiansen OB. Prognosis for live birth in women with recurrent miscarriage: what is the best measure of success? Obstet Gynecol. 2012;119(1):37-43.